The Welfare State and Mother’s Milk
August 10, 2011
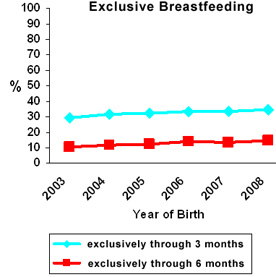
Percent of U.S. children who are exclusively breastfed for three or six months, according to CDC National Immunization Survey
THE FEDERAL GOVERNMENT has sounded the alarm in recent months. The state of infant nutrition in America is in disrepair. A number of reports have been issued, including a “call for action” in January from Surgeon General Regina Benjamin and one just last week from the Centers for Disease Control and Prevention.
An army of facts and numbers has been gathered on the plains of bureaucratic warfare to document a serious public health problem: The vast majority of mothers are not breastfeeding their babies enough.
That this is a public health problem is indisputable. Even to the public health geek, who sees all through the lens of statistics, human milk is irreplaceable. Children are seldom dying without it (the mortality rate attributable to formula feeding involves about 1,000 cases a year), but their well-being in many instances is seriously undermined and the effects have been documented. Ironically, though manufactured formula is costly, low-income parents are much more likely to use it.
What is also indisputable is that the federal government is a major cause of the problem and is seemingly hell bent on keeping it that way.
For all the expense and effort that has gone into the call for action, one would think officials really wanted to see more infants healthy and well-fed. In their heart of hearts they do, but their minds and intentions are clouded by self-interest, political orthodoxy and misguided liberal paternalism. The public effort to encourage better infant nutrition is a window onto the welfare state and its inner workings, a case study in the inability of our federal bureaucracy to overlook its own interests, commercial pressures and ideology on behalf of children.
For the most important and necessary step to improving the incidence of breastfeeding is never mentioned by the Surgeon General or the CDC: The federal government should get out of the business of supplying millions of mothers with free infant formula.
Here are some basic facts.
FACT ONE: Fifty-three percent of the infants in America participate in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) for low-income parents (at or below 185 percent of poverty level). WIC provides free infant formula to any qualifying mother who wants it. A mother does not need to show that she is among the tiny minority (about five percent) of all mothers of infants who are physically incapable of breastfeeding to receive vouchers for formula. About half of the infant formula used in the country is distributed by WIC.
FACT TWO: The total WIC budget is $7 billion.
FACT THREE: The American Academy of Pediatrics recommends that infants be breastfed exclusively for six months and with food supplements for at least a year. Most major health organizations endorse this recommendation.
FACT FOUR: The antibodies and hormones in breast milk are unique and cannot be replicated. They protect infant health and lower the incidence of asthma, gastrointestinal illnesses, ear infections, Sudden Infant Death Syndrome, obesity and Type 2 diabetes. A baby’s risk of becoming an overweight child goes down, for instance, with each month of breastfeeding. (In the US, one in five children under the age of five is at least overweight, and half of these are obese), according to the CDC. Breastfeeding may lower the incidence of leukemia too.
FACT FIVE: Cancer rates are lower in women who have breastfed their children. Breastfeeding is linked with a lower incidence of post partum depression.
FACT SIX: According to the U.S. Dept. of Health, “The nation benefits overall when mothers breastfeed. Recent research shows that if 90 percent of families breastfed exclusively for 6 months, nearly 1,000 deaths among infants could be prevented. The United States would also save $13 billion per year — medical care costs are lower for fully breastfed infants than never-breastfed infants. Breastfed infants typically need fewer sick care visits, prescriptions, and hospitalizations.”
FACT SEVEN: There is evidence that breastfeeding increases maternal sensitivity, widely viewed as an important factor in determining overall childhood health and well-being. This does not mean that a healthy maternal bond cannot occur with a formula-fed infant, but that overall breastfeeding mothers are more attuned to their children.
FACT EIGHT: Only 15 percent of mothers overall adhere to the AAP standard. Half of all infants in the United States have been given formula within the first week of their birth. And only 31 percent are breastfeeding at all by nine months.
FACT NINE: According to George Kent, of the University of Hawaii, “Breastfeeding initiation and duration rates among WIC participants have increased dramatically over the past ten years, but they still lag twenty percentage points behind those of non-WIC participants. This statistic holds true even when controlling for socioeconomic status, geography, race/ethnicity, the age of the mother and birth eight of the baby. In other words, it appears something about the WIC program itself is producing an effect that depresses breastfeeding.”
FACT TEN: Black mothers breastfeed at a significantly lower rate than whites. Only 8 percent of black mothers overall follow the AAP standard. In general , less educated mothers breastfeed less. In former days, wealthy mothers sent their children out to wet nurses. Today, breastfeeding is a hassle for the poor and less intelligent mother who has no economic incentive to breastfeed. She may be put off by the inconvenience of feeding an infant eight to twelve times a day, is not as well read in the health literature and often has less maternal sensitivity to begin with.
IN CONCLUSION, no nation has ever commandeered the basic processes of feeding infants as dramatically as ours has. The free feeding of infants, whatever its good intentions, has institutionalized parental neglect, impoverished health and enriched manufacturers of formula. (See George Kent’s observations on the business interests involved.)
The most important solution to the disastrously low rate of breastfeeding – that the federal government get out of the business of formula feeding – is never mentioned at all in the Surgeon General’s Call to Action to Support Breastfeeding. What we have instead is bureaucrats urging costly measures on the part of hospitals, employers and the federal government to make breastfeeding easier and more appealing, as if breastfeeding should be easy, a pleasure, rather than a mother’s duty and the most economical choice. Many of these measures, such as hospital training of new mothers, are worthwhile and practical in themselves but they place the onus on everyone but the mother. Absent the economic incentive to breastfeed, many mothers are unlikely to see beyond the cultural stigma against breastfeeding among the less educated. The fact is, breastfeeding can be a hassle and is widely believed to create fussier babies. Mothers must have serious motivations in the modern world to persist.
Among the costly measures recommended by the Surgeon General is paid maternity leave for all federal employees, a proposal that would add to the body of laws and regulations discriminating against and undermining the traditional family.
The continuing increase in the numbers of WIC mothers is a reflection of family breakdown. But it is also a reflection of how government is aiding and abetting that breakdown. Free infant formula encourages single motherhood, enabling a woman to get by on her own. Clearly, it would be painful for many thousands of mothers to see this subsidy end. But the government’s interest should be in protecting the rights of the vulnerable over the long term.
Government do-gooders shy away from the language of self-sacrifice. But human milk is one of the things that society owes to the young. It is not something that should be provided purely at the discretion of the mother. At the very least, mothers should not be actively encouraged to turn to formula. According to the Surgeon General’s report:
The decision to breastfeed is a personal one, and a mother should not be made to feel guilty if she cannot or chooses not to breastfeed. The success rate among mothers who want to breastfeed can be greatly improved through active support from their families, friends, communities, clinicians, health care leaders, employers and policymakers.
Mothers do need encouragement and support. But the decision is anything but a personal one. It involves another human being, someone who will one day be a full-grown member of society.
Obviously many mothers have no choice today but to feed with formula. They are single and working. But society should not create the supports that make this more likely. Mothers have the duty to feed their infants well and fathers have the duty to enable them to feed their infants. Infants belong to families, not the State. Mothers should not be required to breastfeed, but they shouldn’t be discouraged from it either with subsidized formula.
The WIC program, begun in 1974, is administered by the Food and Nutrition Service of the US Department of Agriculture. It was authorized by the Child Nutrition Act of 1966. Though it now includes small incentives to breastfeed in the form of bigger food packages for breastfeeding mothers, these are of limited value. It’s time to gradually dismantle its program of free formula.
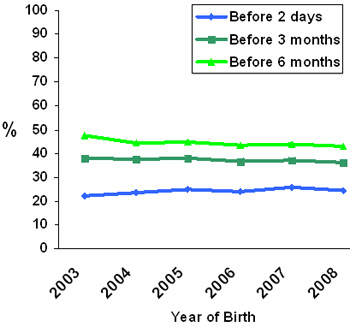
Percent of U.S. breastfed children who are supplemented with infant formula, by birth year. CDC National Immunization Survey.
— Comments —
Lisa writes:
On the subject of nursing mothers and fussy babies: We can see in Victorian-age mothers’ books that it was common knowledge that hassled, distracted, tired mothers did have fussier babies: babies pick up on mothers’ unsettled spirits, and a harried mother can have less rich milk, resulting in shorter periods of feeling satiated for baby. Formula is harder to digest, and leaves a baby sleepier (less “fussy”?) for longer periods of time, another reason that formula would be desirable for working mothers, from a governmental point of view.
And with increasing government attacks and seizures of raw milk sources and animals, even those owned by the milk-consuming infants’ families, infants who only do well with the raw milk, it grows ever clearer that government isn’t truly about “helping” anyone.
Sarah writes:
Your article on WIC and breast milk is wonderful, factual, and well written! I am passing it on to friends and bookmarking it. Thank you for writing this. More people need to be honest about the importance of human milk for human babies. You wrote, “Mothers have the duty to feed their infants well and fathers have the duty to enable them to feed their infants.” This is so true. Wonderfully stated.
Laura writes:
Thank you.
One thing I failed to mention is, it saves a family (without WIC) about $1100 to $1500 a year to breastfeed instead of formula feed. As George Kent notes, some of the high cost of formula, however, is the result of the WIC program.
I was sitting in the dentist’s waiting room yesterday morning when I came across an article by Shirley Wang (it is not available online) in the Wall Street Journal calling for hospital programs to encourage breastfeeding. It was prompted by the latest CDC report and there have been scores of articles like it in other newspapers in the last week. Hospital programs obviously are important, especially given that many women do not have mothers or friends who have breastfed, but I read the statistics in the article and saw the elephant in the room. I came home and later sat at the computer for many, many hours. I was so incensed by what had not been said.
Josh F. writes:
I think the first line of attack in this debate should be against the implicit idea that six months of breastfeeding is even close to being sufficiently healthy for your average newborn. The idea that at a mere six months, a BABY is ready to get off mother’s milk and move on to some imaginary “healthier diet” is pure nuttery.
Traditionalists need to start moving the goalposts, too.
Laura writes:
Actually, the American Academy of Pediatrics does not recommend six months of breastfeeding and then a move to another diet. It recommends six months of exclusive breastfeeding and then the gradual introduction of liquids and solids after that. It also urges continued breastfeeding for at least a year and says nursing is beneficial beyond that. I think those are reasonable guidelines.
Jill Farris writes:
Let’s not lightly pass over the statement that the Woman, Infant, Child program is for “qualifying women.” How hard is it to qualify? Not too hard. Years ago I was urged to get on the program because I “qualified.” I was slightly anemic and “low income” so I took the vouchers for food.
Later, my husband and I watched a news story about what qualified as “low income” for our state and the number seemed very high to us. It was then that we realized that we did not want the government defining poverty for us because they could later use it to justify the many government programs needed to “help” the “poor.” Besides, young families do not need to be encouraged toward self pity and a mindset of needyness. We got off of W.I.C. and when I had days of feeling poor I read stories of the Great Depression to keep things in perspective.
Arual writes:
As a nursing mother I am continually frustrated by the cries of “don’t guilt us!” from moms who either legitimately tried and were unable to feed naturally, or by mothers who didn’t try and want you to validate what they know is an inferior choice, whatever their reasons may be. The former I wish had more support, but I see no shame in doing whatever it takes to feed your baby when breastfeeding doesn’t work out. The latter I am fairly indifferent to, so long as they leave me alone to nurse my child and stop accusing me of immodesty and exhibitionism because I prioritize my child.
I agree with your conclusions about WIC. I applied for WIC a few days after my son was born because I needed help with nursing, desperately, and I had to qualify to gain access to their breastfeeding “warm line.” There are no buts about it, the help I received from WIC peer counselors was superior and ultimately led to the successful nursing relationship I continue with my now 22- month-old son, whereas the hospital lactation consultant I paid for assistance was useless. La Leche League was similarly useless in my valley, it turned out. I have to travel 45 minutes to find leaders who actually meet with women who need help.
In any case, I realized during my struggle that using formula would cost me almost nothing if I went through WIC, and I started the train of thought you have so succinctly presented: subsidizing formula leads to more formula feeding. It needs to stop if the government is serious about improving breastfeeding rates.
Laura writes:
It’s good to know that WIC has helpful lactation counselors.
Hurricane Betsy writes:
Arual complains that “La Leche League was similarly useless.”
La Leche league, a volunteer, mother-to-mother organization, doesn’t represent itself as having numerous trained professional lactation counsellors at the ready, one on every street corner. They are there to help us with the garden variety challenges that countless women face in starting up with nursing our babies. For particularly difficult cases, they do have lactation consultants they can, and do, refer you to. Further, like any other profession, there are mediocre ones and there are excellent ones. So your writer got a “useless” one.
Arual writes:
I was not trying to say that La Leche League in general is useless, merely that the one in my area was. They don’t even have regular meetings anymore, which is distressing and disappointing considering the massive number of new and repeat mothers in the area. We have a very high birth rate here in Utah. I did later gain help from La Leche League leaders, I simply had to drive 45 minutes North to find them. I apologize if it came across that I felt the organization as a whole did a shoddy job. I should have specified that for the area I live in, it is surprising how little help I was able to find.